From Care Pathway Mapping to Data Strategy Implementation
Imagine… you just had a skin cancer spot removed after three rounds of surgery, and the plastic surgeon confronts you with your reflection in the mirror, revealing a large wound on the tip of your nose. However, he then presents you with an AI tool that can simulate a range of reconstructive outcomes. This is a powerful stimulus that better informs you and gives you more autonomy about your treatment choice.
But how do you ensure that a tool like this truly works in everyday clinical practice?
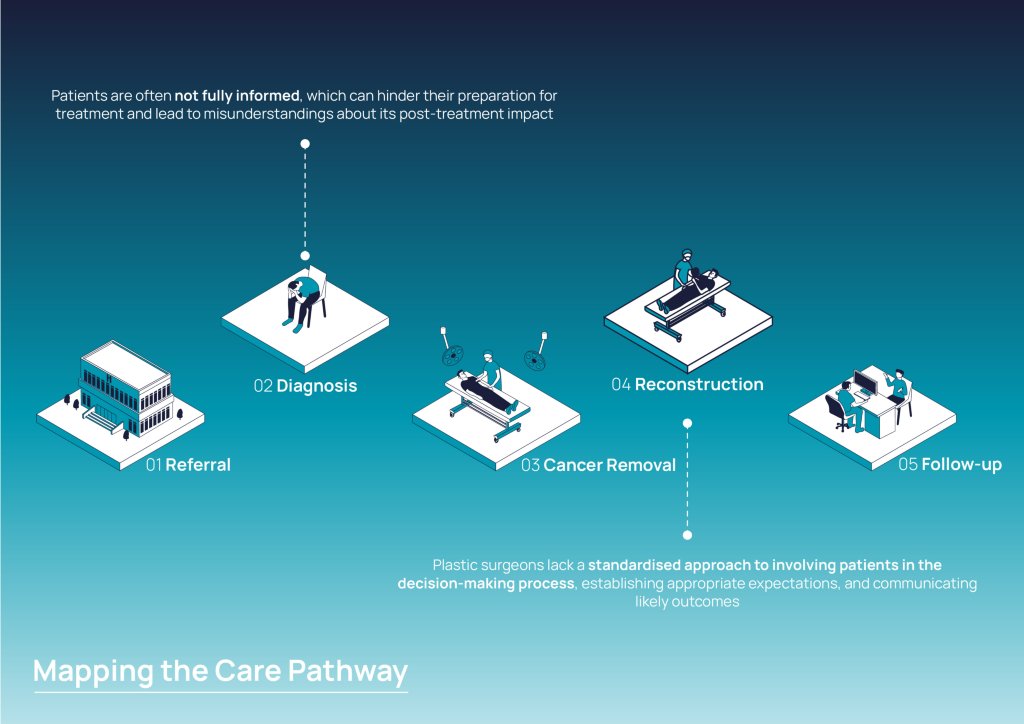
Every day, clinicians have to make complex decisions. While they aim to prioritise what is best for their patient, they often rely on their clinical expertise and personal preferences. Simultaneously, patients often struggle to understand the differences and impact of treatment options. This can lead to a disconnect between patients’ expectations and surgical outcomes, resulting in post-treatment dissatisfaction.
In this project, we explored how AI can help to align patient-physician communication and facilitate shared decision-making by redesigning the care pathway of nasal reconstruction after skin cancer removal.
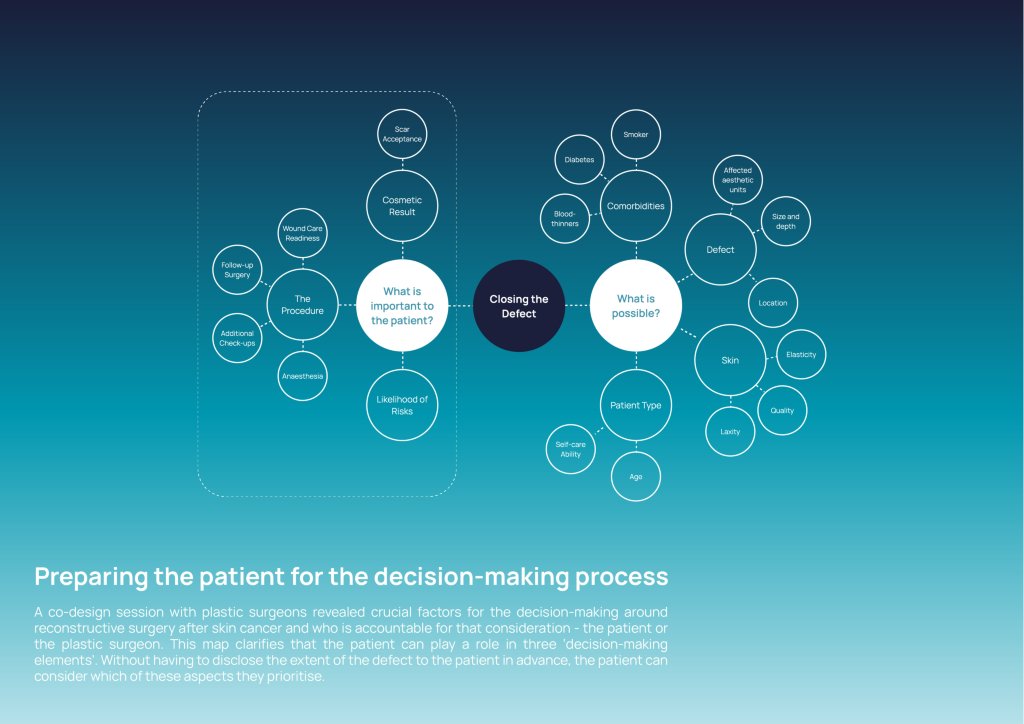
Rather than developing a ‘point solution’, we adopted a holistic approach by combining Multilevel Service Design with the Double Diamond innovation process. Digitising a care pathway requires attention being paid not only to patient-physician interactions but also to non-human actors such as information, software, and data. Within this framework, we redesigned three components of the service system: the value proposition, the technical infrastructure, and the experience.
We mapped the current situation for each component to identify pain points and needs. Technical, clinical, and design stakeholders were involved to co-create future scenarios.
The resulting service solution features a predictive decision-support tool that analyses past cases to match new patients to similar profiles and predict which reconstruction option is most likely to deliver a satisfying result. The tool supports patients when preparing for treatment and helps surgeons communicate outcomes, guiding a more patient-centred consultation.
An additional outcome was the creation of an actionable data strategy to support Catharina Hospital's transition towards more personalised and data-informed care.
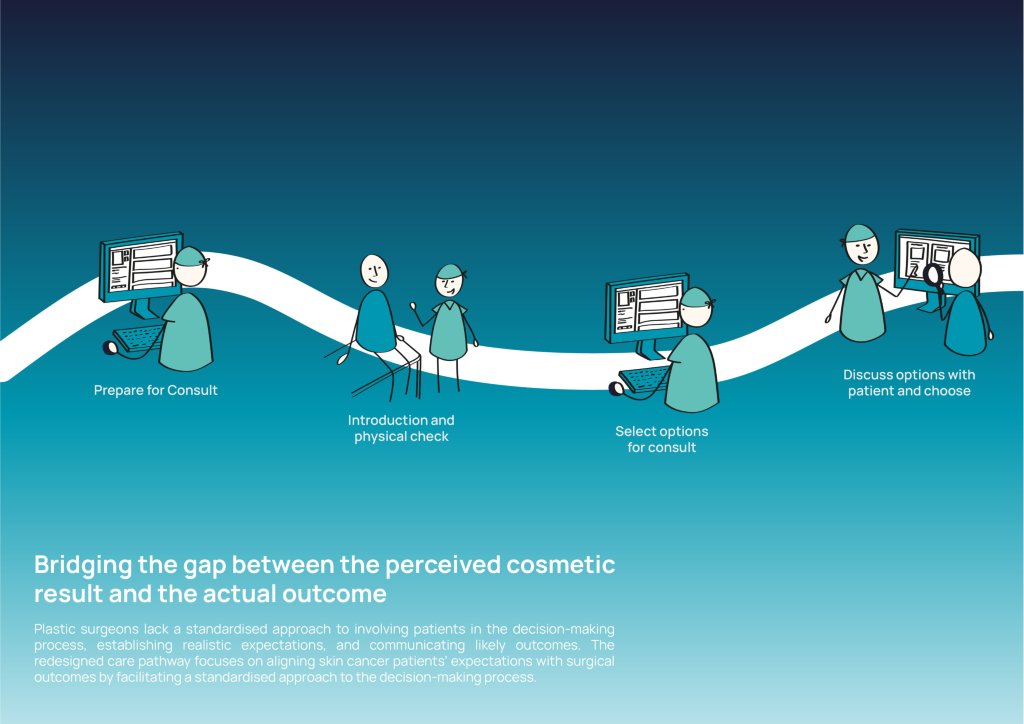

While AI holds great potential to personalise and enhance healthcare, it cannot operate effectively alone. Our project demonstrates that predictive tools only become valuable when we understand how clinicians, patients, and hospital systems have to adapt alongside them. Redesigning the nasal reconstruction care pathway also reveals a broader issue: healthcare data are messy, fragmented, and unstructured, which means AI solutions need thorough preparation before being implementable. For AI to succeed in healthcare, it must be human-centred, supported by collaborative workflows, and built on a strong data infrastructure.
Share
Contacts
- -
